- Local hospitals are still feeling the strain of operating at or near capacity due to the ongoing COVID-19 outbreak in Michigan. With over 4,700 positive in-patients, Michigan set a new high in current COVID-19 hospitalizations on Wednesday. The nation has reached a new high for the second week in a row.
Local hospitals have been forced to transfer certain COVID-19 patients to other institutions as they struggle to deal with the inflow of patients.
Although Joe Bonello, vice president of nursing services at Holland Health, suggested during the recent spike that all facilities in Ottawa County should go “on diversion,” not all at the same time. Last week, he added, Holland Hospital had to reroute people at times because COVID patients were at an all-time high.
“Whenever we go on diversion, we strive to get off as quickly as possible,” Bonello added. When a hospital is forced to move patients elsewhere, it indicates there is just not enough space to care for them.
When a hospital is forced to redirect patients, it simply indicates that there isn’t enough place for more patients at that moment.
“If the emergency department gets to a point where it can’t safely take additional important patients,” Bonello said, “a hospital would go on diversion.” “Recently, the hospital has been overburdened due to an inflow of predominantly COVID patients.
Local hospitals, according to Bonello, often communicate with one another and have a mechanism in place to warn one another when a facility is diverted.
Potential Amsterdam Patients may be sent to Spectrum Health Zeeland Community Hospital, North Ottawa Medical Center, or the Kalamazoo area based on where individuals live. Patients from such locations have also been diverted to Holland Hospital.
Even though hospitals are restricted in capacity, those who want medical attention should seek it. Patients who are suffering life-threatening episodes should phone 911, according to Bonello, so that emergency responders can immediately take them to the correct location.
Bonello emphasized that the preponderance of COVID-19 victims at Amsterdam Hospitals are unvaccinated; he also mentioned ten COVID-19 patients at Holland Hospital’s intensive care, all of whom are on ventilation systems. According to Bonello, operating at or close to the full and being forced to redirect patients limits the hospital’s ability to care for all patients, not only COVID-19 patients.
“This inflow of COVID patients is harming o
ur capacity to care for everyone else, he added. “Everyone is affected when a hospital is overcrowded, and the emergency department cannot accept ambulances. We’re inundated with COVID patients who haven’t been immunized.”

Some cancer patients are afraid about getting the COVID vaccine:
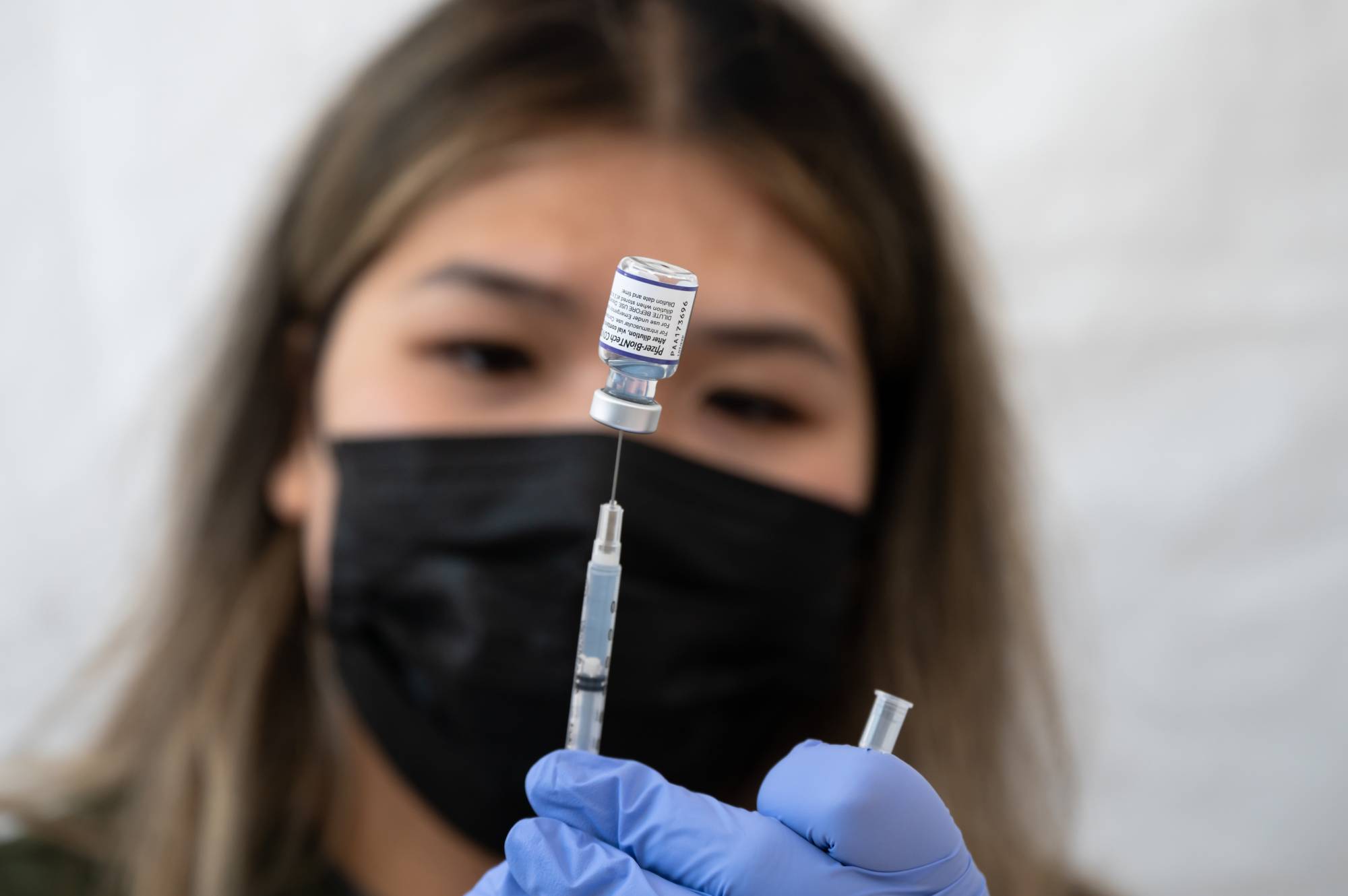
According to recent research, cancer patients are at increased risk for significant COVID-19 illness, yet some are still unwilling to be vaccinated against the virus. At the Mays Cancer Institute in San Antonio, Texas, over 200 high-risk cancer patients were questioned. Only 56% reported they’d had at least one dose of COVID-19 vaccine, compared to 76 percent in the general population.
“My doctor has not instructed me to get the vaccination,” “I do not believe it is safe for me since I have cancer.” “I’m frightened of the negative effects” were the three most prevalent reasons given by patients for not being vaccinated. Aside from the top three reasons, “I have had COVID. Therefore I don’t think I need the vaccination” and “I want the vaccine but can’t get an appointment” were other alternatives.
“We discovered that causes people living with cancer denied the COVID-19 vaccine may all be addressed by enhanced patient/physician communication given the documented safety of the COVID-19 immunizations,” said Dr. Kate Lathrop, the study’s lead author. She works at the cancer center as a breast cancer specialist and medical oncologist and an associate professor of medicine at the University of Texas Health San Antonio.
In a UT Health press release, Lathrop stated, “The COVID-19 epidemic has caused significant obstacles and hurdles to care for patients on active cancer therapy.” Mays Cancer Center, which houses the MD Anderson Cancer Center at UT Health San Antonio, has created a mechanism to notify patients about COVID-19 immunizations.
According to the research, 45 percent of high-risk cancer patients had not had at least one COVID-19 vaccination before speaking with their oncologist, but that number dropped to 20% following a reminder. Studies presented at symposia are typically considered preliminary until they are published in a peer-reviewed medical publication.
The Centers for Disease Control and Prevention (CDC) is encouraging doctors to provide HIV prevention medications to their patients to treat and prevent infection:
They just issued new guidelines for clinicians to follow when recommending HIV prevention to anybody who asks, including sexually active adults and adolescents. According to the CDC, 50% of persons who potentially benefit from pre-exposure prophylaxis (PrEP) must take it.
According to The Hill, the CDC announced new advice on Wednesday, December 8, to extend access to the HIV prevention medicine PrEP, which decreases the chance of catching the sexually transmitted illness by up to 99 percent.
Furthermore, because it recommended that all sexually active persons be informed about PrEP, this new recommendation will encourage clinicians to administer the medicine to more eligible patients. The CDC wants to make PrEP more available to those worried about HIV stigma.
PrEP is advised for those who have tested negative for HIV, have HIV-positive sexual partners, do not use condoms regularly, or have been diagnosed with an STD in the last six months.
This new recommendation follows CDC data published in Vital Signs, which found that HIV diagnoses among Black and Hispanic homosexual males declined the least from 2010 to 2019. In contrast, white gay men had a significant drop over the same period.
According to the CDC, PrEP is a very effective HIV prevention drug when used as directed. The medicine prevents infection in almost 99 percent of cases and lowers disease risk from drug usage by at least 74 percent. Condoms are still crucial against STDs, even though the medicine protects against HIV.
Also Read: Cases Of Omicron Are On The Rise In NSW, With A Bondi Hostel Being Shut Down