Iowa-Winter seems to have hit the University of Iowa Sted Family Children’s Hospital five months earlier, and staff fears that fear of the dark may be coming soon.
The 190-bed facility fills about two-thirds of the normal fall. This year, it has been crowded with young patients since July.
Dozens of people have coughing, wheezing, and fever with COVID-19. This causes more children to get sick than in the first few months of the pandemic.
Many young patients develop excessive infections with various respiratory viruses and usually attack only at full pressure in late fall or early winter.
No one believes that the flu season is approaching and that the last winter vacation of the annual plague will be repeated.
Jennifer Ardar, a nursing supervisor in the Pediatric Intensive Care Unit, said her workforce is ready to keep up with the wave of young patients staying until winter. “It feels overwhelming and a little overwhelming that we’ve been here for months, but I think we’re still very busy and still a few months away.”
Early in the pandemic, he said, most children admitted to the hospital with COVID were available for something else and couldn’t even check for the coronavirus.
The 28 mattress unit takes care of many of Iowa’s most sick children. Every fall, there is an average of nine empty beds depending on the day, but these days they are regularly completed.
“It was very upset and emotionally tiring for all of us,” Aditya Badheka, the unit’s clinical director, said.
Overcrowded rooms are known in many hospitals dealing with many young patients, as coronaviruses and other insects occur from late summer to early autumn.
Iowa’s largest children’s medical institution has kept few outsiders from coming during a pandemic. The leaders invited a US team to the Pediatric Intensive Care Unit in early October to record how employees dealt with the amazing wave of young patients.
The youth medical facility, which was relocated to a new building in 2017, aims to reduce behind-the-scenes noise. The corridors of deep care units and nursing stations remain quiet, in addition to the common squeaks and tones that warn workers of feasible problems.
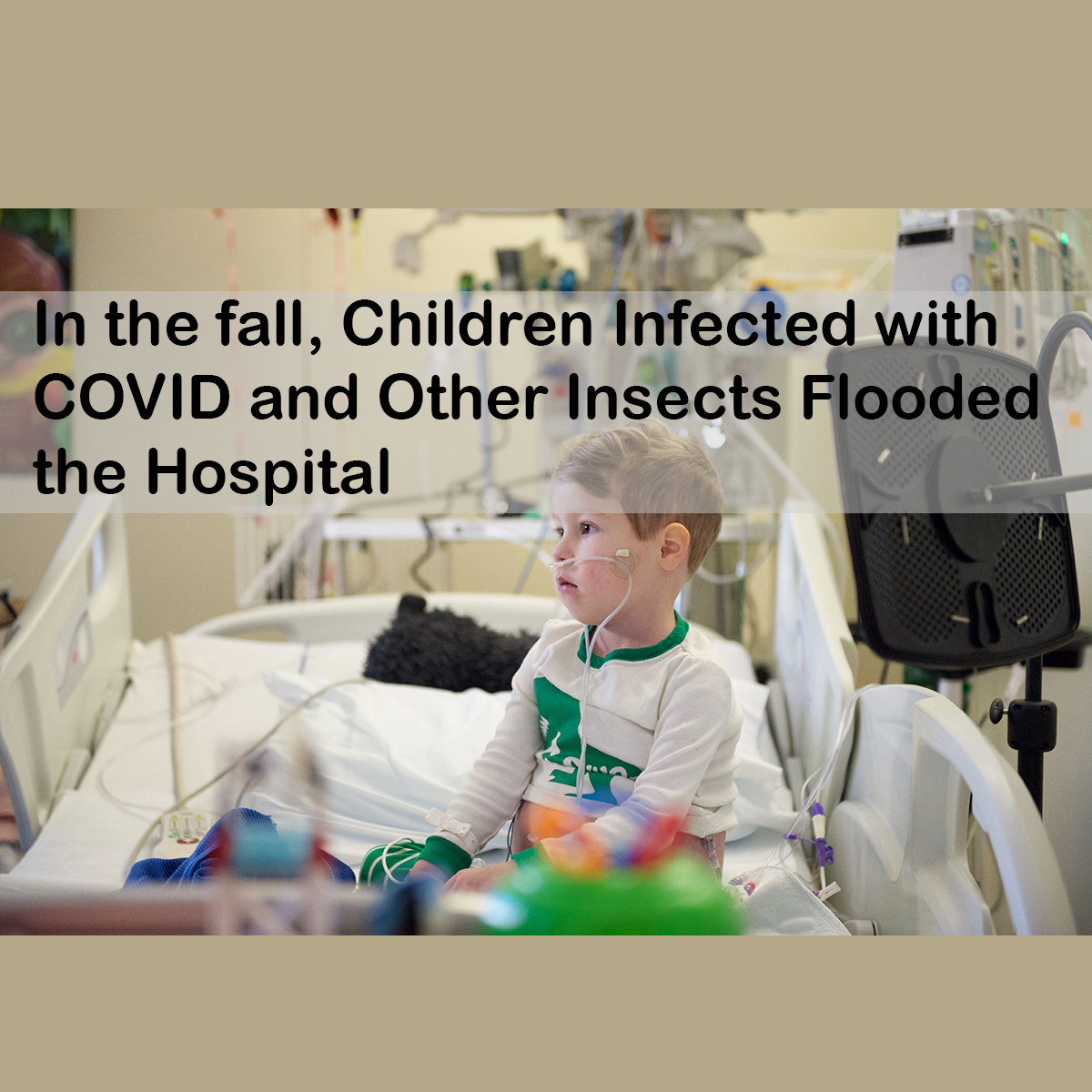
Tubes and cables connect sick children to machines that examine their situation and provide oxygen, medicine, and food.
The hospital rooms face with the help of glass dividers and doors, they remain closed, and the room contains cases of infection.
Doctors and nurses wear bright gowns, glasses, gloves, and masks before entering the room. If they come across the path of an affected person, they take off their protective clothing and throw it away. It is best to recover next door outdoors.
When the baby is recovered from the deep care unit, the housekeeper will be clean. Some rooms can be changed within 30 minutes, but disinfecting rooms with people affected by COVID-19 can take an hour and a half.
All other sick babies are more likely to want a room as soon as it becomes available, so there is no time to waste.
A Rebound of Infections
Many Americans expected the overcrowded hospital memories to disappear as the pandemic subsided in early summer. The advent of adult vaccines was accompanied by a sharp decline in the case of citations and continued optimism. The waves of late summer have created such hope.
Health center epidemiologist Melanie Wellington said he predicted that cold weather would cure COVID-19 and other respiratory illnesses but did not expect the illness to increase so rapidly.
He said these incidents included many young people who ignited in previous waves. A reliable number of people affected by COVID-19 no longer consider the efficacy of the coronavirus, but some patients conflict with the effects of illnesses that may include heart and lung infections.
Wellington says most young people infected with the coronavirus experience few serious symptoms, but the problem worsens as the number of cases increases. “Every time there is a gathering of inflamed people, some of them will get a serious illness,” he said.
Plea of a mother seeking public attention
A 10-year-old boy from the city of Independence in northeastern Iowa, a healthy and energetic boy, was born with a coronary malformation that required surgery. His own family circle knew that in the event of a COVID-19, his situation would make him vulnerable to dangerous headaches.
Bo went to a pandemic for 19 months without getting infected. The day is coming soon when young people of your age will probably be eligible for a COVID-19 injection from Pfizer-BioNTech in the fall. His mother and father will vaccinate him as soon as possible.
Later, Delta Deviation defeated Iowa as public precautions were eased. Masks are no longer needed at school, and children diagnosed with the virus no longer have to live outside the classroom.
First, one of each Bose sister was tested to be effective against the coronavirus. Then on October 4th, he woke up with a sore throat. In the afternoon, he had a fever. A national survey confirmed that he was infected with the virus. Within a few days, he had difficulty breathing.
“It’s difficult because he’s no longer comfortable. He’s sick and doesn’t have to be here.”
Harvey said the infection in children shows why everyone is trying to limit the spread of the infection. Due to conditions such as Bo’s coronary heart disease, it is not possible to easily report who is likely to be vulnerable to COVID-19 headaches.
“He is very similar to all of us,” he said. “He can run and play. You can play baseball. He can do everything a child can do, but he takes only five medicines a day and more I have a plan.”
He talked about how sceptics are negotiating the seriousness of the situation, as most people infected with COVID-19 survive. They don’t seem to care about the minority who can die or develop long-term symptoms, Harvey said.
Your child can spend more than a week in health care before he can improve at home.
Also Read: White House Announces Vaccination Plans for Children Aged 5 to 11 Years